Community based cooking courses have positive effects on fruit and vegetable intake and cooking confidence Lessons from Jamie Oliver’s Ministry of Food
Although government policies often focus primarily on increasing consumer knowledge about healthy eating to improve national diets, individuals are likely to require practical skills to utilise this knowledge. Culinary nutrition is a new approach which combines aspects of nutritional principles with cooking and culinary knowledge in the form of ‘hands on’ cooking interventions often based in the community1. Lack of cooking skills have been associated with poor diet, and increased consumption of highly processed and energy dense convenience food of reduced nutritional quality2,3. Furthermore, households of lower-income often have poor diets and are at greater risks of diet-related diseases4,5, and are least likely to be confident at cooking6.
Jamie Oliver’s Ministry of Food (MoF) campaign aims to reduce diet-related inequalities by teaching individuals how to prepare quick, healthy and low cost home cooked family meals, using fresh ingredients. The impact of the MoF cooking course has been evaluated in the UK in relation to changes in fruit and vegetable (F&V) and snack intake and confidence in cooking, in individuals who attended the Leeds Kirkgate Market centre from 2010 to 2014 (figure 1). In this pre-post intervention study, quantitative outcomes were measured prior to and immediately after the course, and at a six month follow-up. Self-administered questionnaires were used to record the number of portions of F&V consumed per day, number of snacks consumed per day, and participants’ cooking confidence levels (highest score of 5). 795 adults (43% male) were evaluated before and immediately after the course out of 1210 who attended (a response rate of 66%); 462 completed questionnaires at all three time points (a follow-up response rate of 58%). More than double the national average level of deprived individuals were recruited. In addition 40 participants participated in structured telephone interviews providing details of their experiences of the course.

|
Figure 1: Ministry of Food course in Leeds Kirkgate Market, UK Courses provided by ‘Zest Health for Life’ |
Significant increases in mean daily F&V consumption and cooking confidence levels
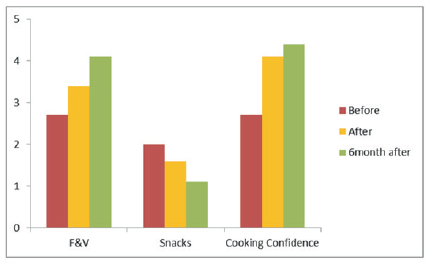
There were significant increases in mean daily F&V consumption and cooking confidence levels and a significant decrease in the frequency of snacks consumed immediately after the course (for those completing questionnaires at a) two time points, N=795 and b) at three time points, N=462). Furthermore, six months after the course self-reported F&V intake had significantly increased from the start of the course by 1.5 (95%CI 1.3, 1.6, p<0.001) portions per day, the number of snacks reported significantly decreased over the same period by -0.9 (95%CI: -1.0, -0.8, p<0.001) snacks per day, and cooking confidence increased over the same period by a score of 1.7 (95%CI 1.6, 1.9, p<0.001) out of five (figure 2).
|
Figure 2: Changes in F&V intake, snack intake and cooking confidence before, immediately after and 6 months after the Leeds Ministry of Food cooking intervention (N=462) |
Multivariate regression analyses showed that age and disability, but not deprivation or ethnicity, were associated with changes in self-reported F&V intake and cooking confidence scores between the start of the course and six months afterwards. Younger adults (16-19) had significantly smaller increases in F&V intake of around half a portion compared to the 20–64 year olds (difference between groups −0·60 (95% CI −1·10, −0·10) portions/d, P=0·02) and those with physical impairments had a smaller change than those with no disabilities (−0·69 (95% CI −1·32, −0·07) portions/d, P=0·03). Smaller increases in cooking confidence were reported for younger adults than older, and for those with learning disabilities than those with no disabilities. Furthermore, males reported a greater increase in cooking confidence scores at six months after the course than females (0·29 (95% CI 0·04, 0·55) increase, p=0·03).
The results of the telephone interview supported quantitative findings. Respondents said the course had improved their knife skills, use of seasoning and aspects of food hygiene as well as other core cooking skills. They also reported an increase in awareness of shopping costs, budgeting and a greater awareness of healthy food access within Leeds market. Many participants said they visited the market more, having an increased awareness of the healthy food available to them there. For participants from deprived areas of Leeds the most valuable aspect of the course seemed to be learning new recipes and ways to cook from scratch using basic ingredients, with most participants from these areas learning healthier ways to cook which included using less oil and fat, while just under half-gained knowledge about the value of fresh ingredients. Participants also reported eating less frozen, processed and takeaway foods high in fat. A key benefit for participants of the course was socialising with others on the course – for example, some participants with disabilities or living in deprived areas reported a clear decrease in social isolation.
MoF community based cooking interventions can have significant positive effects on cooking confidence and food choice, specifically F&V and snack intakes
They may encourage short-term changes in dietary behaviour which can be maintained and improved over longer periods of time. They can also produce a wider range of social outcomes, including an increase in selfefficacy, personal control and general confidence in adults. Communitybased cooking interventions may present an effective mechanism to facilitate positive dietary changes without widening socio-economic inequalities.
Based on: Hutchinson J., Watt J. F., Strachan E. K., & Cade J. E. Evaluation of the effectiveness of the Ministry of Food cooking programme on self-reported food
consumption and confidence with cooking. Public Health Nutrition, 19 (18), 3417-3427 (2016)
References
- Condrasky MD & Hegler M (2010) How culinary nutrition can save the health of a nation. J Extension 48, 2COM1.
- Brunner TA, van der Horst K, Siegrist M (2010) Appetite 55, 498-506.
- Hartmann C, Dohle S, Siegrist M (2013) Appetite 65, 125-131.
- James WP, Nelson M, Ralph A et al. (1997) BMJ 314, 1545.
- Darmon N, Drewnowski A (2015) Nutr Rev 73, 643-660.
- Adams J, Goffe L, Adamson AJ et al. (2015) Int J Behav Nutr Phy Act 12, 99.
