Inequities in obesity and obesity-related behaviours: A priority for policy-making
Socioeconomic position (SEP) refers to individuals’ social and economic position in relation to others’ and is often measured by assessing income, education and/or occupation1. Individuals with a lower SEP are more likely to be obese and to have poorer dietary and physical activity behaviours relative to those who are more advantaged2,3. Given that obesity and obesityrelated behaviours are associated with increased risk of chronic disease4, their socioeconomic patterning may partly explain why disadvantaged groups have a higher risk of chronic disease. These health differences are referred to as health inequalities/inequities.
Universal vs. targeted policies to reduce obesity and improve obesity-related behaviours
Two main types of policies have been used to address health inequities. Targeted policies aim to address determinants of health in the most disadvantaged groups (e.g. food vouchers for low-income groups), whereas universal policies are aimed at the entire population (e.g. nutrition labels on pre-packaged foods)5.
In a previous systematic review we found that the majority of universal policies had no impact on inequities in obesity and obesity-related behaviours6. This article describes findings from a second systematic review in which we synthesized evidence from controlled studies pertaining to the impact of targeted policies on anthropometric, dietary and physical activity outcomes amongst socioeconomically disadvantaged children and adults. To be included in this systematic review, studies had to be published between 2004 and 2015, evaluate the impact of a policy targeted at disadvantaged individuals in a developed nation, include a control group, and report an anthropometric, dietary or physical activity outcome.
Organizational policies
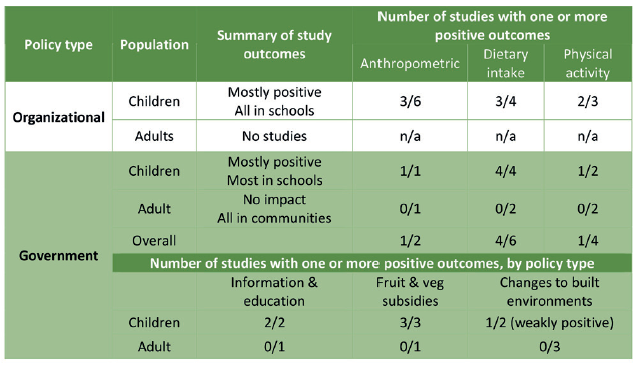
Eight studies assessed the impact of organizational policies implemented as part of 7 distinct multi-component interventions in disadvantaged schools. Six of the 7 interventions were effective.
Studies reported a greater impact on dietary and physical activity behaviours than on anthropometric outcomes. Common elements of successful policy-containing interventions included nutrition standards for foods and beverages, enhancements to physical education classes, additional physical activity opportunities, school self-assessments, and teacher, child and parental nutrition and physical activity education. Given the multi-component nature of the interventions, it was not possible to attribute any positive impacts to policy specifically.
Evidence from government policies
Ten studies assessed the impact of single-component government policies in disadvantaged children and/or adults. Government policies were less successful in changing physical activity relative to dietary behaviours, with only two studies examining anthropometric outcomes. Three broad types of policies were examined: 1) Provision of information/education; 2) Fruit and vegetable subsidies; and 3) Changes to built environments.
The first two policy types showed evidence of effectiveness in disadvantaged children, but not in disadvantaged adults. Changes to built environments were not effective in disadvantaged children or adults. Caution is warranted, however, as there were only 2-4 studies of each policy type.
The importance of interventions in childhood to reduce obesity and improve obesity-related behaviours
This synthesis of evidence from controlled studies found the largest quantity of high quality evidence of effectiveness for comprehensive interventions that included school policies, and government policies targeting socioeconomically disadvantaged children in schools. No studies evaluated the impact of organizational policies directed at disadvantaged adults, whereas all government policies assessed in this review that targeted disadvantaged adults proved ineffective. These findings highlight the importance of focused interventions in childhood to ameliorate the negative obesity-related manifestations of low SEP, along with gaps in knowledge pertaining to effective policies in community settings and in adults.
Table: Summary of study results
Based on: Olstad DL, Ancilotto R, Teychenne M, Minaker LM, Taber DR, Raine KD, Nykiforuk CIJ, Ball K. Can targeted policies reduce obesity and improve
obesity-related behaviours in socioeconomically disadvantaged populations? A systematic review. Obes Rev 2017;18(7):791-807. https://onlinelibrary.wiley.com/
doi/abs/10.1111/obr.12546 Copyright © [2017, World Obesity Federation]
References
- Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health 2006;60(1):7-12.
- Global strategy on diet, physical activity and health. World Health Organization, 2004.
- A systematic review of studies on socioeconomic inequalities in dietary intakes associated with weight gain and overweight/obesity conducted among European adults. 2010;11(6): 413-29.
- Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks 1990–2015 a systematic analysis for the Global Burden of Disease Study. 2016;388(1659-1724).
- Health inequalities: concepts, frameworks and policy. London: Health Development Agency, 2004.
- Olstad DL, Teychenne M, Minaker LM, Taber DR, Raine KD, Nykiforuk CI, Ball K. Can policy ameliorate socioeconomic inequities in obesity and obesity-related behaviours? A systematic review of the impact of universal policies on adults and children. Obes Rev 2016;17(12):1198-217.
