Practical advice on the role of diet in treating patients with Irritable Bowel Syndrome

Irritable bowel syndrome (IBS) affects the digestive system and can substantially impact quality of life. More than 80% of patients with IBS associate their gastrointestinal symptoms with eating food (Bohn, 2013).
The present article is an expert review of the American Gastroenterological Association (AGA) in order to provide best practice advice statements, primarily to clinical gastroenterologists, covering the role of diet in IBS treatment (Chey, 2022).
Referral to a registered dietitian nutritionist is recommended for most irritable bowel syndrome patients
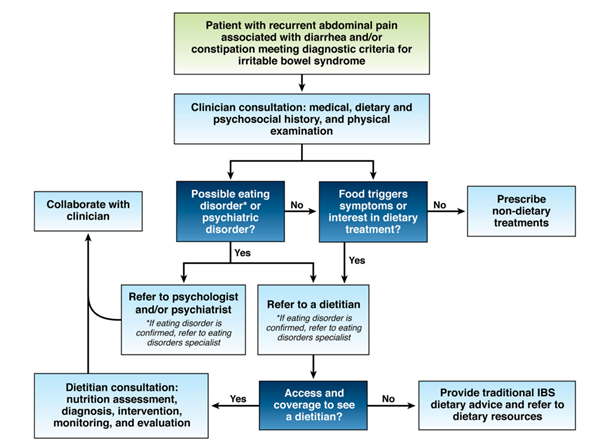
Most patients with IBS associate their gastrointestinal symptoms with eating food. The first recommendation for these patients is therefore to refer them to a registered dietitian nutritionist for dietary advice if 1/ they have insight into their meal-related gastrointestinal symptoms, 2/ they are motivated to change their diet, 3/they wish to collaborate with a dietitian and 4/ they do not have an eating disorder. Restrictive diet interventions for patients at risk for malnutrition and those who are food insecure are not recommended (figure 1).
When setting up an appointment with a dietitian, the clinician and patient should provide previous medical and demographic information, including test and procedure results, biochemical data and anthropometric data. It is recommended that patients keep a food diary for at least three days and a corresponding symptom chart prior to their appointment. Ongoing communication and collaboration between the treating physician and the registered nurse is crucial to ensure that the patient’s care plan is aligned and optimized.
Even if a low FODMAPs diet can reduce the symptoms, it should always be monitored by a dietician
The most common macronutrients found to trigger IBS symptoms are carbohydrates. In particular, FODMAPs are short-chain, poorly digestible and poorly absorbed sugars that can trigger symptoms in some patients with IBS. It has been found to reduce overall and individual symptoms in randomized controlled trials.
A meta-analysis including 7 randomized controlled trials showed a significant reduction in symptoms when comparing a low FODMAP diet and other interventions in 397 people with IBS (Dionne, 2018). A more recent meta-analysis confirms these results and the efficacy of this diet in the short term to relieve overall symptoms, abdominal pain and bloating (Black, 2021). It appears that short-term FODMAP restriction has little impact on micronutrient intake and overall diet quality could even be improved if the patient is monitored by a dietitian (Eswaran, 2020; Staudacher, 2020). However, studies have limitations related with their methodology, such as lack of blinding and small sample size.
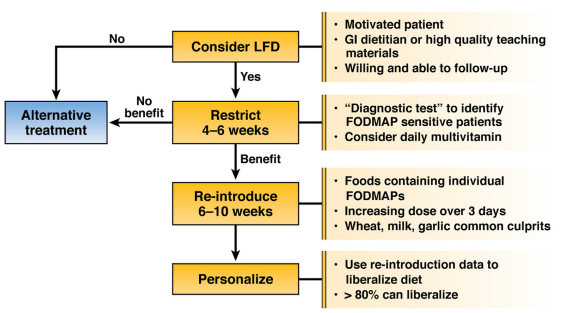
Multiple clinical trials have shown that a 4-6 weeks of low-FODMAP diet is sufficient to determine whether a patient with IBS will respond (Dionne, 2018). This short duration reduces the risk of complications related to excessive food restriction, which can lead to long-term eating disorders (McGowan, 2021). As described in figure 2, the low-FODMAP diet is divided into 3 phases:
- restriction during 4–6 weeks,
- reintroduction of FODMAP foods,
- personalization based on results from reintroduction.
Healthy eating advice are also beneficial for some patients with IBS.
Soluble fiber is efficacious in treating global symptoms of irritable bowel syndrom
Dietary fiber is a carbohydrate not absorbed or digested in the small intestine. We distinguish between soluble fiber and insoluble fiber whose consumption does not have the same effect on patients with IBS. A systematic review and meta-analysis of 15 randomized controlled trials showed that soluble fiber may have positive impact on patients with IBS. Conversely, insoluble fiber can increase bloating and abdominal pain. Therefore, 2021 American College of Gastroenterology Guidelines on the management of IBS recommends the use of soluble fiber for the treatment and improvement of global IBS symptoms (Lacy, 2021).
Regarding a gluten free diet, there is a lack of strong evidence supporting the efficacy of this diet in relieving IBS symptoms. Further efforts to identify and validate biomarkers that predict response to dietary interventions are needed to deliver “personalized nutrition.”
Based on: Chey WD, et al. AGA Clinical Practice Update on the Role of Diet in Irritable Bowel Syndrome: Expert Review. Gastroenterology. 2022 May;162(6):1737-1745.e5.
All of the best practices recommended by the American Gastroenterological Association (AGA) Clinical Practice Update (CPU) are listed below:
- Referred to a registered dietician nutritionist.
- Routine screening for disordered eating or eating disorders by careful dietary history is critical because they are common and often overlooked in gastrointestinal conditions.
- Specific diet interventions should be attempted for a predetermined length of time. If there is no clinical response, the diet intervention should be abandoned for another treatment alternative, for example, a different diet, medication, or other form of therapy.
- In preparation for a visit with a RDN, patients should provide dietary information that will assist in developing an individualized nutrition care plan.
- Soluble fiber is efficacious in treating global symptoms of IBS.
- The low-FODMAP diet is currently the most evidence-based diet intervention for IBS.
- The low-FODMAP diet consists of the following 3 phases:
1) restriction (lasting no more than 4–6 weeks),
2) reintroduction of FODMAP foods, and
3) personalization based on results from reintroduction. - Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results.
- There are limited data showing that selected biomarkers can predict response to diet interventions in patients with IBS, but there is insufficient evidence to support their routine use in clinical practice.
